For Patients
WHEN DO I SEE AN OPHTHALMOLOGIST?
Even if you have not experienced eye problems in the past, you should see an ophthalmologist if:
- you experience a change in vision in one or both eyes, such as blurring, double vision, blind spots, flashing lights or floaters
- your eyes experience pain, persistent irritation, itching, discharge or the sensation of a foreign body
- you have had recurrent conjunctivitis, or red eyes
- you experience problems with too many or too few tears
- you are currently taking steroids orally for any other condition
- you have a growth on the eyelid or the eyelid is incorrectly positioned
- you are diabetic
- you are aged above 40
- you have a family history of glaucoma
INPATIENT PROCEDURES
Accomodation Facilities
Patients who require surgery or monitoring will be asked to get admitted in the hospital. Patients can choose from the different types of rooms based on the availability. At the time of counseling, the counselors will assist you in selecting the room, surgical techniques and implants available. Based on your convenience, you can choose the package of your choice. Cashless facilities and reimbursement certificates can be availed as applicable. Many of the surgeries are being done as day care procedures. Patients undergoing day care procedures need not stay in the hospital after the surgery. The package charges vary based on the type of accommodation selected for procedures other than the day care. Following are the different types of accommodation facilities available:
- Suite
- Private Rooms
Payment
On admission, a deposit equivalent to or approximate to the treatment or surgery charges will be collected. The balance if any, will be collected / refunded at the time of discharge based on the surgery / treatment and the type of accommodation chosen. Bills are payable by cash, with insurance claims, if any. Credit and Debit cards are accepted with applicable charges, if any.
Discharge Procedure
Patients are requested to vacate the room before 10.00 am on the day of discharge. Instructions regarding post operative care, medication, discharge summary will be explained by the ophthalmic assistants at the time of discharge.
Support Services
Catering services
Cafeteria is located on the ground floor and is open from 7.30 am – 8.00 pm. Breakfast, lunch and dinner are available there.
Medical shop and Optical shop
General Instructions
Visitors
The hospital solicits co operation for maintaining quiet ambience. Children are strictly not allowed to visit or stay with the patient.
Security instructions
You are advised not to bring valuables to the hospital. Do not hand over money and valuables to strangers. The incharge ward nurse available can be approached for further details. Closed circuit camera’s are provided in the hospital for the safety of patients. For further assistance, contact Hospital Administrators who will be available from 8.30 am- 5.30 pm
OUTPATIENT PROCEDURES
Eye Examination Procedures
There are many different eye conditions; you will need to have a detailed eye examination which could take upto 2 hours, depending on the complexity of tests required. The durations indicated below are an average.
Registration
On arrival you will be asked to fill in a registration card. Please give your complete permanent address with telephone number.
You will be asked to take a seat until our receptionist accompanies you to your vision test.
If the patient is below 15 years, you will be taken directly to the Paediatric ophthalmology.
Vision test
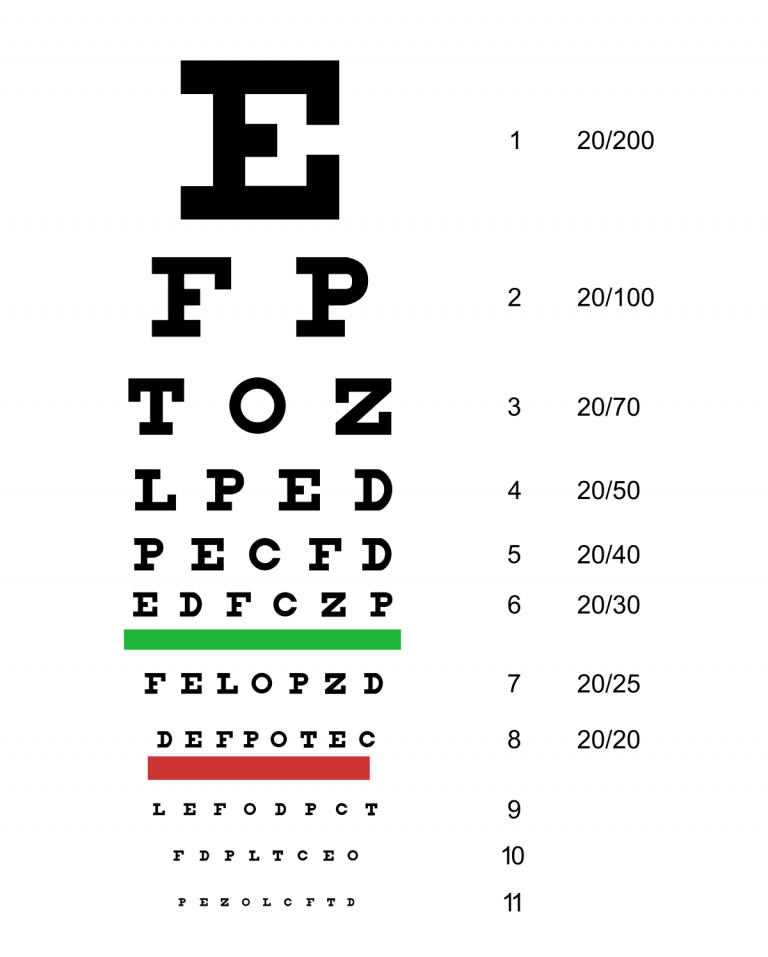
Every patient has a simple test to check your level of vision from an eye chart.
Refraction
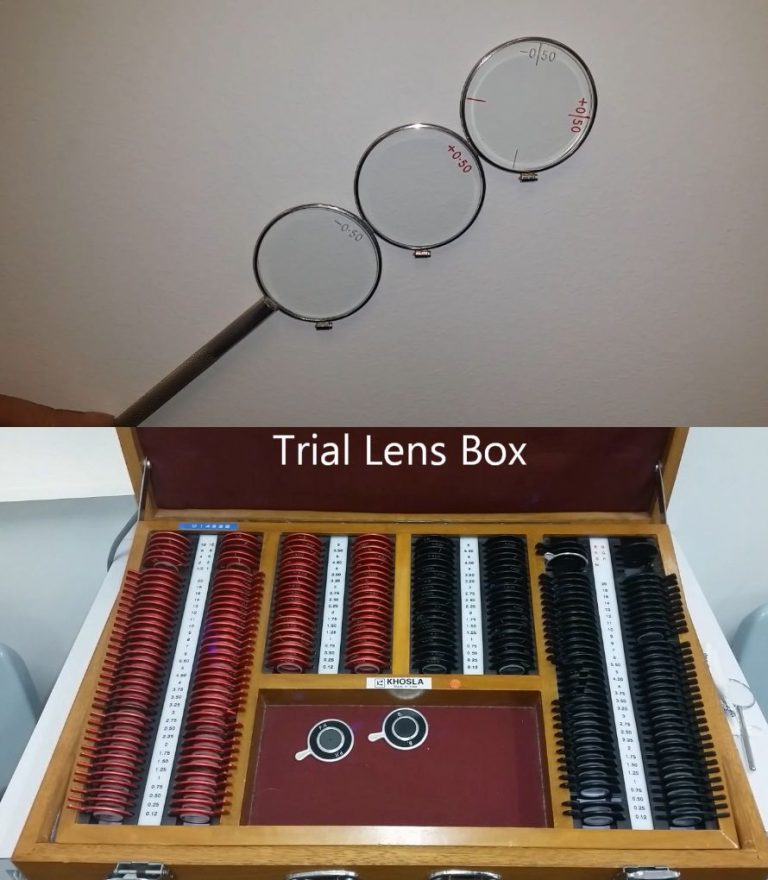
A refractionist will place a series of lens in front of your eyes and will ask which looks clearer. This test determines your exact eye power and determines your level of sight.
Preliminary examination
An eye doctor will carry out an initial examination of your eyes, please advise the doctor of any previous medical history. Blood pressure / Eye tension / Sugar test ( 30 minutes) This is only for patients aged 40+, we will check your blood pressure, intraocular pressure and a urine test for diabetes. Stages 3 – 5 may happen in any order depending on the patient load.
Dilation
The doctor in some cases may ask the refractionist to instil eye drops in the eye. This is to make the pupils bigger in order to get a better view of the inside of the eye. It may take 30 minutes for dilation, you will be asked to wait in the waiting room during this time. You will experience blurred vision for 2 – 3 hours following dilation. Final examination and diagnosis After all the tests have been carried out the doctor will carry out a final examination and depending on the results you will be guided to the speciality clinics.

What is Ophthalmology?
What is the first step?
At our Hospital, the diagnosis of the eye problems starts with a detailed physical examination and assimilation of medical and genetic history. It is followed by specific tests such as:
Subjective Refraction Determination: Using a reading table of letters, numbers and symbols displayed on a screen, the visual acuity of the eye is determined. If the visual acuity does not meet the required standards, corrections are made using corrective lenses placed in an individual frame.

Click on link to read more
Cataracts are a degenerative form of eye disease in which the lens gradually becomes opaque and vision mists over. Depending on the extent of the disorder, surgical intervention is recommended.
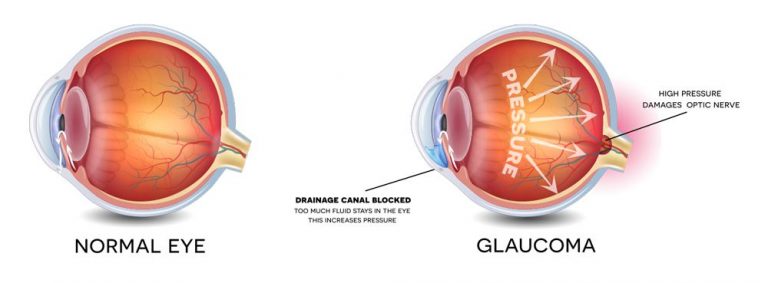
Glaucoma occurs when a build-up of fluid in the eye creates pressure, damaging the optic nerve. Once this disorder is detected, steps such as prescription eye drops, lasers or even surgery is recommended to prevent the problem from progressing and leading to blindness.
Squint corrective surgery is often recommended in most cases. Squint measurements and if need exercise are advised initially.
Dry eye management is recommended to prevent the eye from drying out, thus ensuring that the eye is well moisturised. Corneal ulcers and allergies are managed and treated. Minor surgeries for Pterigium is undertaken. Our specialist handles Corneal Suture and Corneal Scrapping as well.
The Medical Retina helps to diagnose, monitor and treat the conditions that affect the lining of the back of the eye, called the retina. Common conditions include age related macular
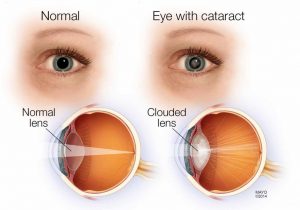
CATARACT
A cataract is formed due to clouding of the area around the lens of the eye. It blocks the passage of light into the retina. Hence, it causes problems in vision. Mostly, the cataract develops slowly without disturbing the eyesight in early stages. But over a period, it does disrupt the eyesight.
Causes of Cataract
One of the most common causes of cataract is age related. The build-up of proteins in the lens, which makes it cloudy. It prevents the passage of light to retina causing vision problems.
Cataract can also be caused due to genetic disorders, diabetes, trauma, long term use of steroids and past eye surgery.
Types of Cataract
The types of cataracts include age-related cataract, congenital cataract, secondary cataract and traumatic cataract.
Age-related cataract: It is caused due to aging.
Congenital cataract: In some cases, children maybe born with cataract due to poor development or an injury or an infection.
Secondary cataract: It is caused as a result of medical conditions like diabetes, exposure to UV light, radiation and so on.
Traumatic cataract: It is caused post an eye injury.
Several other factors that increase the risk of cataract include excessive drinking, cigarettes smoking and air pollution.
Symptoms of Cataract
Cataract symptoms include:
Dim, clouded or blurred vision, fading of colours, Double vision in affected eye, Problem with light and glare, Visualizing a halo effect around a light source
Diagnosis of Cataract
The doctor diagnoses cataract by reviewing the medical history, signs and symptoms as well as an eye test which include visual acuity test, slit lamp examination and retinal examination.
Visual acuity test: A reading test, that helps determining the reading ability.
Slit lamp examination: A test conducted using slit lamp, that helps diagnosis. The ocular structures are magnified using the slit lamp.
Retinal examination: A test conducted using dilating drops, to examine the retina.
Treatment of Cataract
The treatment of cataract mainly is surgical.
The doctor may recommend wearing eyeglasses or contact lens, if the vision can be corrected non-surgically. But if the vision cannot be corrected with the help of eyeglasses or contact, the doctor may recommend a cataract surgery.
Glaucoma
Glaucoma is a group of eye conditions characterised by damage to the optic nerve, which is vital to vision. This damage may be assisted with abnormally high pressure in your eye.
Glaucoma should be treated at the right time, because vision loss due to glaucoma cannot be reversed. The key to this is to have regular eye exams, and check for eye pressure. The maximum that can be done to treat glaucoma once a patient has it, is to slow down the process and the resultant blindness.
Symptoms of Glaucoma
Depending on the type and stage of glaucoma, the symptoms are divided into:
Open-angle glaucoma symptoms: Typically, symptomless until in advanced stage
Tunnel vision in the advanced stages. Patchy blind spots in the side (peripheral) or central vision frequently in both eyes
Acute angle-closure glaucoma symptoms
Severe headache, Halo around lights, Eye pain, Eye redness, Nausea, Vomiting, Blurred vision
Risk Factors of Glaucoma
A person may be at a higher risk of getting glaucoma with the following conditions:
Has high internal eye pressure. Increasing age typically from 40 years, maybe earliest in African descent. Has a family history of glaucoma. Has existing medical conditions such as diabetes, heart disease, sickle cell anaemia, high blood pressure, has existing eye conditions such as near-sightedness, has oestrogen deficiency for example when both ovaries are removed before age 43. Has been taking corticosteroid medication such as eye drops for a long time. It has been observed that population originating from Cuba, Mexico, Puerto Rico, South America or Central America and the Sub Saharan Africa have a higher risk of developing Glaucoma
Diagnosis of Glaucoma
In order to diagnose glaucoma, the doctor will review the patient’s medical history and conduct complete eye examination. This will include tests such as:
Checking for optic nerve damage, measuring intraocular pressure (tonometry), Measuring corneal thickness (pachymetry), Checking for areas of vision loss (visual field test), Inspecting the drainage angle (gonioscopy)
Treatment of Glaucoma
The damage caused by glaucoma can’t be reversed. But treatment and regular checks can help slow or prevent vision loss, especially if detects the disease in its early stage. The following treatment may be given to control glaucoma:
Medication:
These include eye-drops such as prostaglandins, beta blockers, Alpha-adrenergic agonists, Carbonic anhydrase inhibitors, Miotic or cholinergic agents.
If the eye drops do not work, the doctor may prescribe oral medication as well. This is usually a carbonic anhydrase inhibitor.
Surgery:
Laser trabeculoplasty is an option for people with open angle glaucoma.
Filtering surgery is the removal of part of the trabecular meshwork.
Drainage tubes is the inserting a small tube in the eye.
In case of acute angle-closure glaucoma, the patient will need urgent treatment to reduce the pressure in the eye. This generally will require both medication and laser or other surgical procedures.
